
There are many diseases that manifest as painful sensations in the lumbar region. They can indicate problems with the spine, joints, muscles, internal organs - kidneys, intestines, liver. This is a very insidious symptom and without a visit to the doctor it is impossible to determine the true cause of the pain in the lumbar region. Proper treatment is possible only after diagnosis in a medical institution.
Types of pain
During the initial examination, the doctor should ask the patient about the nature of the pain. In duration they can be:
- sharp- occur suddenly, paroxysmally, vary in intensity, last less than 1 month;
- subacute- they last 2-3 months, most often they are repeated: they are activated for 2-5 days, then calm down and return again after some time;
- CHRONIC- last more than 1 year, the course is most often repeated.
Doctors have found that more often chronic pain in this area is associated with the formation of local muscle spasms, compressions that have specific pain points (the so-called myofascial syndrome). The process also involves the muscles that guide the spine, gluteal muscles, pelvic ligaments, and the sacroiliac joint.
The nature of the pain is sharp, aching, dull. By intensity - strong, medium, weak. Depending on the location of the pain, the following types are distinguished:
- lumbodynia- pain in the lumbar or lumbosacral region;
- sciatica- in the lower back, radiating to the legs;
- sacralgia- in the area of the sacrum;
- coccidinia- in the tail.
5 facts about back pain
- About 25% of all visits to clinics with complaints of back pain are related to sensations in the lumbar region.
- According to research, 84% of people have experienced pain in the lumbar region at least once in their life.
- 44-78% of patients (depending on age and region of residence) experience repeated attacks of lumbodynia.
- Up to 37% of people periodically lose their ability to work due to low back pain.
- In 85% of patients who consult a doctor for pain in the lower back, musculoskeletal disorders are identified, which become the cause of the pain.
- According to statistics, about 90% of patients with acute pain in the lumbosacral region recover within 2 weeks.
Causes of back pain
Musculoskeletal disorders
In 2006, the European Federation of Neurological Societies officially adopted the following classification of the causes of pain in the lower back. They are divided into 3 main groups:
- Compression of the spinal root, peripheral nerve in the lumbar spine. It occurs due to the elongation (degenerative changes) of the intervertebral discs. Less often, due to dysplasia (disorders in the formation process) of the upper articular processes of the sacrum.
- Diseases of the spine caused by tumors, joint injuries, infections, compression fractures, allergic reactions, autoimmune inflammatory processes.
- Musculoskeletal disorders as a result of subluxation, sprain of spinal ligaments, muscle strain, dysfunction of intervertebral joints.
Pathologies of internal organs
- Disorders of the genitourinary system.
Diseases of the urinary system - urolithiasis, cystitis, pyelonephritis - often cause discomfort in the lumbar region.
Back pain in women may indicate dysfunction of the genital organs. Most often, the main sensations are concentrated in the lower abdomen and radiate to the sacrolumbar spine. They can appear during menstruation or after sexual intercourse.
One of the possible causes of back pain in women are ovarian tumors, which are located at the back of the uterus. Often, discomfort in the lower back becomes a symptom of uterine fibroids. As it grows, the pain can appear strong and acute and indicate serious disturbances in the blood supply, stretching of the peritoneum and compression of the nerve plexuses in the pelvic area.
Another cause of back pain in women is pelvic organ prolapse. In this case, the sensations are of an attractive nature. During walking and physical work, their intensity increases.
- Disorders of the gastrointestinal tract.
Most often, pain is felt in the lumbar region due to gastric and duodenal ulcers and acute pancreatitis. Patients complain that there is pain of generational character. Usually the lower back starts to hurt simultaneously with the right/left hypochondrium, where the most intense sensations are concentrated. In a number of clinical cases, lower back pain accompanies the attack of acute appendicitis, although it is not the main symptom of this disease. Various inflammations of the intestinal mucosa (proctitis, sigmoiditis) can also cause pain.
10 risk factors for back pain
- Congenital pathologies of the lumbosacral spine.
- Heavy physical work accompanied by stress on the lower back, frequent bending and vibration.
- Acute and chronic stress that causes muscle spasms.
- A sedentary lifestyle and prolonged standing in an unnatural position with a load on the lumbar region.
- A weak muscular corset, which results in poor posture, stooping, scoliosis and kyphoscoliosis.
- Metabolic disorders and excess body weight, which increases the load on the lower part of the spine.
- Increased physical activity and participation in sports increase the risk of injury.
- Age over 50 years - due to the development of degenerative processes in the spine.
- Frequent stress, depression.
- Poor nutrition with a lack of B vitamins.
Back pain as a symptom of various diseases
Osteochondrosis of the lumbar spine
One of the most common diseases, the symptom of which is pain in the lumbar region. With osteochondrosis, the intervertebral discs, which play a shock-absorbing role between the vertebrae, become thinner. Nerve roots are compressed, muscles spasm, and severe acute pain occurs. Its intensity increases when bending, lifting heavy objects or when the patient tries to sit down from a lying position or get up from a sitting position.
In advanced cases, a hernia is created between the vertebrae, which only adds to the pain. Osteochondrosis most often affects the lumbar spine, as it bears the maximum load when sitting and walking.
A serious complication of osteochondrosis is spondylosis. It is characterized by the almost complete destruction of the intervertebral discs and the formation of sharp bone protrusions - osteophytes. They damage nearby tissues, causing sharp, severe pain that radiates down one or both legs.
Signs of intervertebral hernia
- The patient can rise from a sitting position only with support from a chair/table or knee.
- Any load on the lower back causes an attack of acute pain.
- The patient lies on his stomach, placing only a pillow under him.
- A person can pick up an object from the floor just by bending slowly.
Ankylosing spondylitis
The disease appears as a result of inflammatory processes in the spine. It is most often diagnosed in men aged 20-35 years. The patient feels stiffness in the lower back and discomfort in the sacrum in the morning and at rest. Gradually, during the day this feeling passes, the person "step by step". Many people do not pay attention to this alarming symptom; meanwhile, ankylosing spondylitis leads to gradual fusion of the vertebrae, decreased mobility of the spine, and disability. Therefore, you should see a doctor at the first signs of the disease - morning stiffness in the spine.
Spondyloarthrosis
This disease affects the cartilage tissue that covers the intervertebral discs. With age, it becomes thinner, destroyed, and bony growths form in the places where it breaks. Due to the fact that the intervertebral discs rub against each other, the nerve roots are irritated - this process is accompanied by severe back pain. The muscles in the problem area of the back are constantly tense and spasm.
Signs of spondyloarthrosis
- The pain gets worse after exercise and goes away after rest.
- Pain appears after long standing or walking.
- Simultaneously with the lower back pain, the patient feels discomfort in one of the hips and the hip joint.
Urolithiasis disease
The pain in this pathology is paroxysmal and very intense. Typically, painful sensations arise from an inflamed kidney. It is difficult for the patient to find a position in which he feels better. After the attacks, the urine takes on a reddish color and its volume decreases.
Inflammation in the superficial tissues and fibers
The cause of the pain may be a carbuncle or boil. These are dense purulent formations on the skin with a diameter of more than 1 cm. They are easily spotted by their purple color. Painful sensations are sharp, intense, pulsating.
Paranephritis, an inflammation of the perinephric tissue caused by infection, is also painful. Sensations become stronger with inhalation and movement. The patient tries to lie with his legs folded - in this position the pain is less pronounced. The skin in the affected area swells and becomes red.
Inflammation of the spine, spinal cord
Osteomyelitis is an inflammatory process in the bone marrow that affects all bone tissues. The acute form is characterized by increasing pain of a pulling, explosive nature. It is combined with signs of intoxication and fever.
Tuberculosis of the spine occurs due to infection with Koch's bacillus. The first signs of the disease may appear many years after infection. It all starts with deep pains that appear after training. The infection affects the vertebrae, hindering the patient's movements and a characteristic gait is formed.
Other diseases
Lumbar pain can be a symptom of many pathologies, including quite exotic ones. These include, for example, foot and mouth disease, Ebola fever, hemorrhagic fever and Japanese mosquito-borne encephalitis.
- Cardiovascular diseases - aneurysm of the abdominal aorta, Loeffler's endocarditis.
- Myositis is inflammation and muscle pain in the lower back, which can be caused by infectious diseases such as flu, sore throat and even common ARVI.
- Benign and malignant neoplasms of the spine and spinal cord.
- Renal pathologies - glomerulonephritis, thrombosis of renal veins, pyelonephritis, cyst.
- Back pain in men occurs with prostate cancer.
Why does my lower back hurt when I cough?
Coughing provokes muscle tension in the affected area, resulting in pain. Often, patients first learn about a developing disease when they notice pain when coughing. Most often, such sensations are a sign of:
- intervertebral hernia,
- osteochondrosis,
- neuralgia,
- facet arthropathy,
- kidney diseases.
Diagnosing

As mentioned above, pain in the sacrolumbar region can be a symptom of many diseases. Therefore, to identify the objective causes, you should consult a doctor at the first signs. You can make an appointment with an orthopedist, neurologist or surgeon. In the future, you may need to consult a rheumatologist, urologist or gastroenterologist.
- Initial examination.The doctor evaluates tissue sensitivity, muscle function and reflexes in the affected area.
- Radiography.The examination shows changes in the structure of bones, cartilage and joints.
- Blood and urine tests.With their help, you can determine the presence of infection and inflammatory processes.
- Functional diagnosis.It includes methods for assessing nerve conduction and muscle performance - electroneurography, electromyography.
- CT and MRI.It allows a detailed examination of the condition of bones, muscles, nervous and vascular structures.
- ULTRASOUNDperformed if pathology of the pelvic organs, prostate or kidneys is suspected.
It is important to exclude (or confirm the presence of) a tumor, to distinguish between spinal root compression and pain syndrome of a musculoskeletal nature. Based on the diagnostic data, the doctor will determine the true cause of the pain and prescribe an effective treatment program.
Is bed rest necessary?
None of the recommendations for the treatment of back pain in diseases of the musculoskeletal system contain instructions for strict bed rest. On the contrary, patients are advised to return to normal activity as soon as possible to prevent the formation of chronic pain syndrome. Strict immobilization is advisable for 1-3 days in severe cases, that is, with severe pain. For acute pain in the lower back, you can use a fixation belt. However, long-term lumbar fixation is not recommended unless there is trauma or spondylolisthesis. You should gradually include special exercises to strengthen the spine and muscles.
Back pain treatment
Most often, a combination of medicinal and non-medicinal agents is required to solve the problem.
Treatment
The basis of drug therapy is non-steroidal anti-inflammatory drugs (NSAIDs). They affect the peripheral mechanisms of pain formation and are prescribed for the aggravation of the pain syndrome. In most clinical cases, treatment is carried out in courses - no more than 12 weeks.
In most cases, patients are prescribed B vitamins to improve nerve conduction, decongestants and sedatives. In the chronic course of the disease, it is possible to take antidepressants. For severe muscle spasms and pain - muscle relaxants, weak opioids.
Non-drug
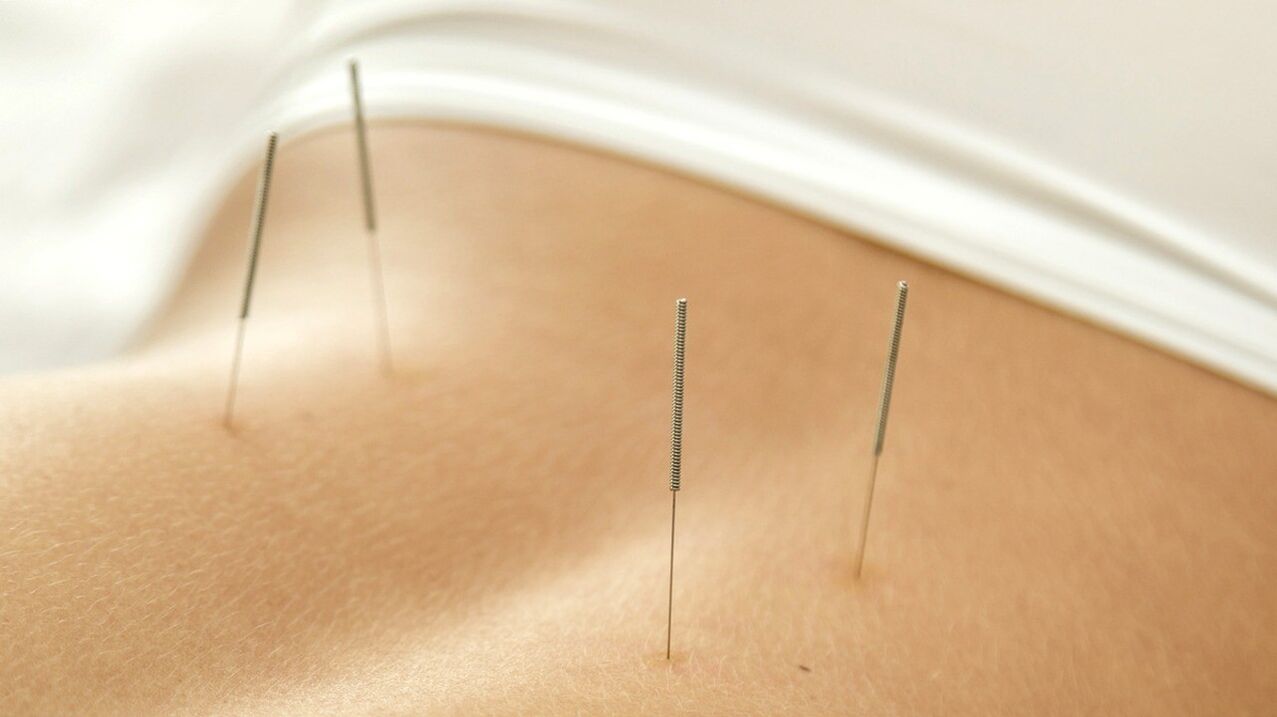
In addition, the patient may be prescribed manual therapy, acupuncture (acupuncture). The procedures are aimed at activating metabolism and blood circulation in the affected area. This enables improved tissue nutrition.
According to doctors, physical therapy, exercises to strengthen the muscles of the lumbar region, traction therapy and transcutaneous electrical neurostimulation have little effect. Most often, these procedures are prescribed in the absence of a pronounced effect from taking drugs for 4-6 weeks. There is no scientific evidence for the effectiveness of massage, physiotherapy or the application of various belts.
What should be done for prevention
- In the morning, exercise with simple stretching exercises for the spine and muscles.
- Eat rationally, excluding fatty, fried, smoked, salty, spicy and alcohol.
- Watch your weight.
- Drink at least 1. 5 liters of fluids (preferably water) a day.
- Once every 6 months, take a classic massage course.
- Avoid staying in one position for a long time.
CONCLUSION
Painful sensations in the lumbar region can be a symptom not only of pathologies of the musculoskeletal system, but also of internal organs. Many patients self-diagnose and treat, for example, a muscle strain, although the problem may actually be inflammation of the kidneys. Such treatment only worsens the situation - a person focuses on a non-existent disease and causes a serious pathology. That is why it is important to seek qualified help and identify the real cause of the pain. Self-prescription of drugs is not strictly recommended.
















